If IR and DR were to separate, I would be very concerned about the long-term implications for the House of Radiology as a whole. A significant amount of administrative, operational, professional advocacy, and negotiation leverage would be lost forever. As the adage goes, united we stand, divided we fall.
More than 400 diagnostic and interventional radiologists signed onto a virtual Town Hall organized by ACR and SIR to address a rising conflict that is currently roiling a specialty squeezed by a workforce shortage—DI and IR: Better Together…or Not?
Held on December 6, a panel composed of IRs and DRs from both academia and private practice—including SR CEO and Chair Scott Bundy, MD, FACR— provided their wide-ranging personal perspectives on the issue and addressed questions submitted by the audience. The Town Hall was co-moderated by the very able Michael D. Dake, MD, Sr. VP, Health Sciences, University of Arizona, and Brent Wagner, MD, MBA, director, American Board of Radiology.
While IR has seriously considered breaking away from diagnostic imaging in the past, the union is currently facing a perfect storm with a newly established, exclusively interventional training track; a significant workforce shortage in radiology; and particularly onerous reimbursement cuts on the interventional side.
Dr. Dade explained that the ACR and SIR recognized the need to address this “elephant in the room” as a growing number of IRs call for IR to separate from DR based on charges that DRs:
• fail to value what a successful IR practice can bring to a radiology practice;
• have not or are unwilling to adapt business models to support the IR practices;
• continue to support the use of exclusive contracts, which create practice barriers for IRS; and
• do not view the practice of IR to be equally important as the DR practice.
The panelists represented both interventional and diagnostic radiology, academia, private practice, and an entrepreneurial model, each articulating their response to the question: Bulent Arslan, MD, FSIR, chair, interventional radiology, Rush University; Mary Constantino, MD, FSIR, an IR, CEO and owner of several office-based laboratories, Portland, OR; James Brink, MD, FACR, chair, Radiology, Massachusetts General Hospital;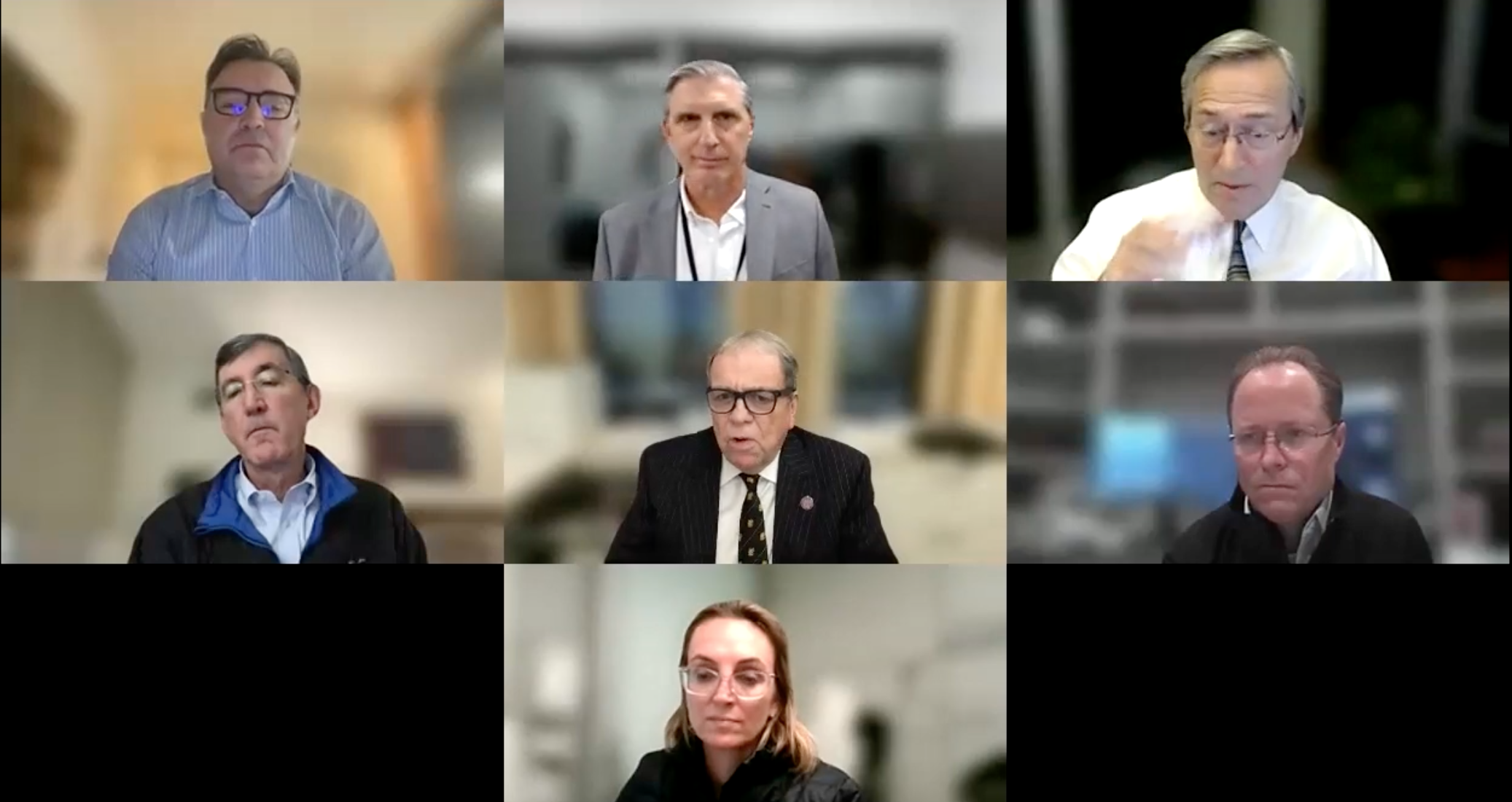 Scott Bundy, MD, FACR, neuroradiologist, Radiology Associates of North Texas; and David J. Spinosa, MD, Fairfax Radiology Associates, VA.
Scott Bundy, MD, FACR, neuroradiologist, Radiology Associates of North Texas; and David J. Spinosa, MD, Fairfax Radiology Associates, VA.
Bulent Arslan, MD: The IR Chair
Dr. Arslan runs the vascular service at Rush Network Medical Center, Chicago. The IR service line began separating from diagnostic radiology in operation, research, budget, and residency training three years ago and was completed two years ago. “That’s why I am here, to support that view,” said Dr. Arslan, a passionate IR. “I think this is inevitable in the future, and I hope it happens with the support of DR, with both specialties backing each other as allies under the hospital roof as well as under the roof of the ACR for larger political strength.”
Dr. Bulent has worked in four settings during the past 20 years, beginning with UVA and including his latest tour with Rush. Acknowledging that IR practice patterns are variable, he identified one constant: “If you establish a robust clinical IR practice, this promotes growth and helps protect turf. If you have a clinical program, even your competing specialists will grow to respect you and start referring cases to you.”
Dr. Bulent maintains that a DR chair will rarely understand, know, or be willing to go to the mat to ensure what is needed to develop a true clinical practice with continuity of patient care. His practice at Rush began with three rooms, three IR attendings and three IR fellows 12 years ago. Today, the service is about to get a seventh room, and the department has seven faculty members and 27 IT trainees. Junior residents take night call and senior residents take pager call, with most patients admitted directly through the IR service by an attending IR physician. The department is developing an outpatient IR lab and working on creating a dedicated interventional oncology clinic at the cancer center.
“In my opinion, the best way to have the IR field…grow and prosper and be recognized by general medical field and the public, is to allow IR to practice independently to become a true specialty,” he said.
James Brink, MD, FACR: The DR Chair
Dr. Brink planted his flag at the outset: “I believe we are stronger together.” He has been an academic chair for 21 years, 10 years at Yale and 11 years at Massachusetts General Hospital, with oversight of radiology at Brigham and Women’s Hospital and ten other specialty and community hospitals in the past two years. MGH operates three physician-owned imaging centers and a physician-owned OBL at its flagship center, with more OBLs planned. Dr. Brink began his statement with a confession.
“We rarely make a mistake if we answer the question at hand from the patient’s perspective,” he began. “Based on that perspective, a few months ago I reached the conclusion and announced to my IR leaders that I felt I had underinvested in IR longitudinal care. I asked my IR leaders to propose ways in which we could increase the scope of our pre- and post-procedural care so that we could offer the same level of service that procedural services offer.”
Nonetheless, having an OBL or investing in longitudinal IR care is not counter to the idea that IR and DR are stronger together, Dr. Brink said, because:
• Scale matters and together IR and DR have more opportunities to help each other
• A strong IR service brings cachet to the DR service.
• DR brings cachet to a combined department particularly with its ability to garner resources from the hospital on behalf of IR and DR services.
• The science of radiology has tremendous overlap between imaging and image-guided intervention.
On this last point, Dr. Brink was quite clear: “One of my colleagues at MGH has developed AI-based robotics for image acquisition with ultrasound, but also image-guided intervention with ultrasound that automatically cannulates the femoral artery and femoral vein,” he said. ‘I worry that if we start carving things out, the science of our discipline will fragment, and we won’t be able to get the advances that we can leverage because of the ability to address imaging and image-guided intervention in the same breath.”
Scott Bundy, MD, FACR: Private Practice Coalition Leader & Neuroradiologist
As one of the architects of a merger that produced the 275-radiologist private practice Radiology Associates of North Texas, and also a practicing neuroradiologist and CEO and Chair of Strategic Radiology, a coalition of 37 independently owned private radiology practices, Dr. Bundy championed the principles that have fueled the success of both organizations: the ability and willingness to listen, transparency, patience, and a culture of teamwork.
He advocated for applying those same principles to ensure that diagnostic and interventional radiology move forward together. “There is no reason that similar principles would not work in making sure that both interventional and diagnostic radiology are more valuable together than if they were separate,” he said. “DRs and IRs have much more in common than they will ever have in common with hospital administrators, entrepreneurial non-physician OBL or imaging center owners, third-party payors, practice consolidators, and even referents."
An exceptionally large, subspecialized practice, RANT operates on an individual role-based model, with each practitioner, whether an IR, a pediatric radiologist, or mammorgrapher, focused on their role in making the practice thrive. In response to the current workforce shortage, RANT tries to be as flexible as possible in crafting the “role” to the applicant, and those conversations take place very early in the interview process. “If somebody is coming out and wants to do nothing but IR, we would look at current needs across the practice to see whether or not they can be plugged into that role,” he said
Dr. Bundy characterized the prospect of a separation of DR and IR as one of dire, deep, and irreversible loss. “If IR and DR were to separate, I would be very concerned about the long-term implications for the House of Radiology as a whole. A significant amount of administrative, operational, professional advocacy, and negotiation leverage would be lost forever. As the adage goes, united we stand, divided we fall.”
Mary Costentino, MD: Entrepreneurial IR
Dr. Costentino owns an OBL in Portland, OR, that she opened with a partner whom she subsequently bought out. “I guess you would say I'm the CEO, chief medical officer, CFO, COO, facilities manager, and the practicing doctor,” she said. Dr. Costentino employs a vascular surgeon and a physician’s assistant, and opened a second center, an OBL/ASC, three hours away, where IR, vascular surgical, and interventional nephrology procedures are performed. She identifies more closely with vascular surgeons than she does with the diagnostic radiologists in a hospital.
“I didn’t necessarily plan this route,” she said. “I was in a group that had the traditional problem of working 80 hours a week and looking at my board and doing ports and permacaths.” In 2011, she decided to go it alone. Now she answers to no one, is financially independent, and doing more complex procedures than she ever did in the past.
Although Dr. Costentino is a solo practitioner, she has experience with many of the radiology groups in Portland and has seen IRs and DRs separate because DRs tired of supporting IRs.
“That’s a common concern, that DRs are subsidizing IRs. I frankly don’t have a lot of patience for that—you’re either all on the same team or you are not, but once you start to have the mindset of we-are-supplementing-you, what you are really saying is, ‘We don’t want to support you.’ If you are going to work together, you’re going to have to value what each other brings to the table. So my final answer is, it depends. It depends on the group, it depends on what you’re trying to get out of it, it depends on who has the relationship with the hospital.”
Value your physicians, all of them, Dr. Costentino urged. “The patients and the doctors are the only people who bring money through the health system—everybody else takes it away,” she said. If a practice declines to optimize interventional opportunities because IR professional fees are going down, Dr. Costentino has a response: “I’m going to throw up an OBL right down the street and make sure we collect technical fees too.”
David Spinosa, MD: Practice President & IR
Dr. Spinosa is an IR and the practice president of Fairfax Radiological Associates in Fairfax, VA. The practice operates three IR clinics, an OBL, an outpatient vascular lab, and co-owns 18 outpatient diagnostic centers in a joint-venture environment. He has practiced in both academic and private practice settings and believes IR and DR are stronger together for the following reasons.
It’s personal for Dr. Spinosa. His experience in working with a 105-radiologist practice which functions as a team has been wholly satisfying, and he attributes its success to the development of a cooperative, constructive relationship between IRs and DRs and other specialties built around common goals. As a cultural matter, FRA emphasizes that the group comes before the section and that the group and the section supersede the individual. Politically, the practice zealously protects its exclusive contracts but collaborates via committee with other specialties within the hospital that are interested in doing imaging and image-guided interventions to make sure everyone shares the same quality measures and equitably takes call. “It’s not for everybody,” he said.” It’s group-think. If you're not in group-think, you’re probably not going to like our practice.”
A clear-eyed view of the financial realities of medicine and radiology contributes to Dr. Spinosa’s position. “Our IRs recognize that finances matter, and we work to be financially responsible to the group,” he noted. “There’s no getting around the fact that money is an important part of the business of radiology.” Dr. Spinosa believes that the number one reason 70% of U.S. physicians are employed and that solo practitioners and small groups struggle to survive is finances.
Finally, Dr. Spinosa believes that there are very few true entrepreneur physicians in the IR community. “Those are very special people among us,” he said. “I think that it is very important that we ask ourselves—when we consider whether we want to be apart or together—a series of questions: How hard do I want to work? Do I want to be a proceduralist or do I want to be a patient’s physician (those are two very different jobs)? How well do I know my local politics (meaning, am I really going to get to do what I want to do or will I have to do what I'm told I'm going to do)? How well do I know my professional finances? As IRs, we can cultivate our practice and be financially sustainable within our practice so that our whole group gets the advantage of us and what we bring to the group”
Changing Hearts and Minds
Pre- and post-event polls that assessed whether Town Hall attendees believed IR and DR are better together showed very little difference, suggesting that few minds were changed on a question with serious ramifications for the future of the specialty. However, the healthy exchange of ideas provided much food for thought, some great advice, and, for blended practices, some excellent intelligence on where the landmines are located. The hope is that groups will walk away from this exchange with greater motivation to form a more perfect union lest their IRs feel compelled to break off and compete.
Hub is the monthly newsletter published for the membership of Strategic Radiology practices. It includes coalition and practice news as well as news and commentary of interest to radiology professionals.
If you want to know more about Strategic Radiology, you are invited to subscribe to our monthly newsletter. Your email will not be shared.