Up to a third of Lisfranc injuries are missed at initial presentation, and it’s a problem. Missed Lisfranc injuries result in chronic pain, disability, mid-foot arthritis, and certainly a lot of litigation.
Residents and seasoned radiologists lucky enough to attend the 2022 meeting of the RSNA were treated to a cringe-inducing selection of MSK, abdominal, chest, and cervical spine trauma cases, all with the potential to show up in the queue for those taking night call, during a Tuesday afternoon session titled, “On-Call Primer for Residents: Don’t Miss Diagnoses.”
Said Laura Avery, MD, moderator, presenter, and thoracic and emergency radiologist at Massachusetts General Hospital: “This is a session intended to give you some pointers on how to navigate some tricky trauma targeted to residents who are taking those night calls. We’re hopeful that we’ll bring you a little bit more confidence. As the surgeons say: ‘Sometimes right, sometimes wrong, but always confident.’ We want you to establish dominance over our trauma surgeons and bring them some excess knowledge.”
This article is based on the first presentation by Ashwin Asrani, MBBS, associate professor of radiology and emergency radiology section chief at Cornell University/New York Presbyterian Hospital, who explored “Tricky MSK Trauma That Keeps You Up at Nght.”
“Is musculoskeletal trauma tricky?” he began. Referencing the Workman’s Compensation Claims Database, he shared that non-spine musculoskeletal is the second largest cause of malpractice claims after breast. “If you combine the spine injuries with the non-spine MSK injuries, this is actually the largest group of malpractice claims,” Dr. Asrani said. “It is definitely tricky for residents and attendings.”
Dr. Asrani cited multiple factors that contribute to the difficulties:
• insufficient or inadequate radiographic views (axillary view lacking, overlapping anatomy);
• presence of non-displaced fractures such as osteoporotic pelvis with ground level-fall;
• common pitfalls in certain sites, such as missing a proximal fibular Maisonneuve fracture;
• little avulsions that portend big trauma, like as a Segond fracture, which is an actual capsular avulsion portending an ACL injury;
• and finally, the satisfaction of search.
He proceeded to walk attendees through a series of five don’t-miss diagnoses in the ED composed of posterior shoulder dislocation, scaphoid fracture, Lisfranc fracture, Maissoneuve fracture, and compartment syndrome.
Posterior Shoulder Dislocation
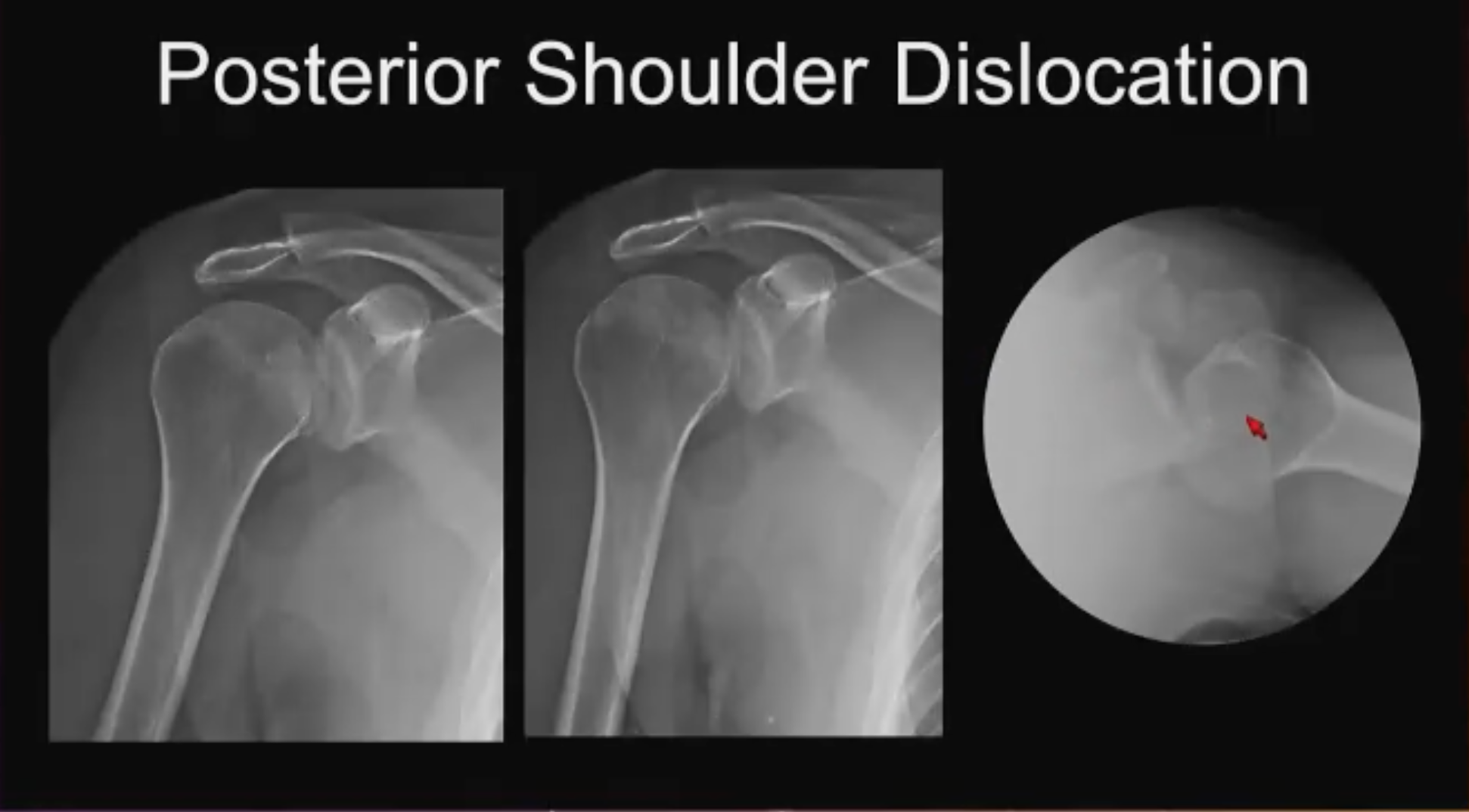
Posterior Shoulder No. 1 (above). Status post-fall. Dr. Asrani reminded attendees that classically posterior shoulder dislocations tend to occur where there is abnormal myoelectrical activity like seizures or electric shocks, where there is asymmetric force or contraction around the shoulder. He said: “ However, the majority of posterior shoulder dislocations are from falls when the humerus is internally rotated, and the arm is adducted. If you look at this cursorily in the middle of the night and don’t have much time, you might think there is no fracture, no dislocation, this is fine, until you get the axillary view.”
“The humeral head is dislocated posteriorly,” he continued. “It is not articulating with the glenoid and it is in fact impinged on the posterior glenoid, essentially a reverse Hills-Sach deformity. Note the little line on the medial aspect of the humeral head, also known as the trough sign, present on both views: the trough sign of posterior dislocation.”
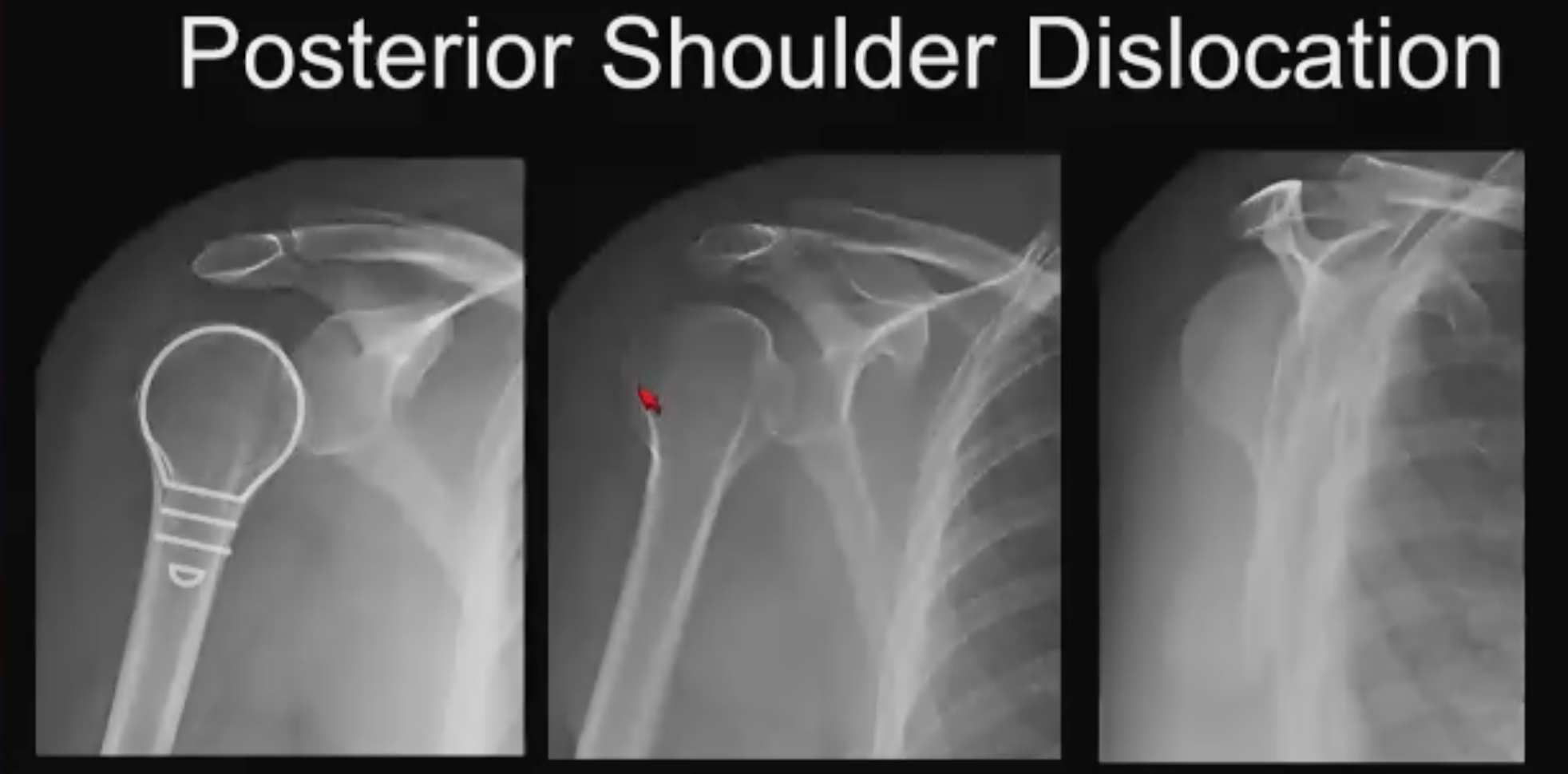
Posterior Shoulder No. 2 (above): No trough sign. On casual review this case looks completely normal. Said Dr. Asrani: “I don’t see a trough sign, there is no sign of fracture or dislocation until I get to the “Y” view. On the Y view the glenoid sits at the center of the Y but the humeral head is posteriorly offset with respect to the glenoid, raising antennas. There could be something going on here, but the Y view can be tricky and there are false positives.”
Going back to the AP views, both the internal and external rotation views, the humeral head has a lightbulb appearance, which is typically the appearance on internal rotation. Said Dr. Asrani: “In other words, the humeral head is stuck in internal rotation. That should tip you off to the presence of posterior shoulder dislocation. In real-life, this was missed completely in a poly trauma case so the patient got a CT. Obviously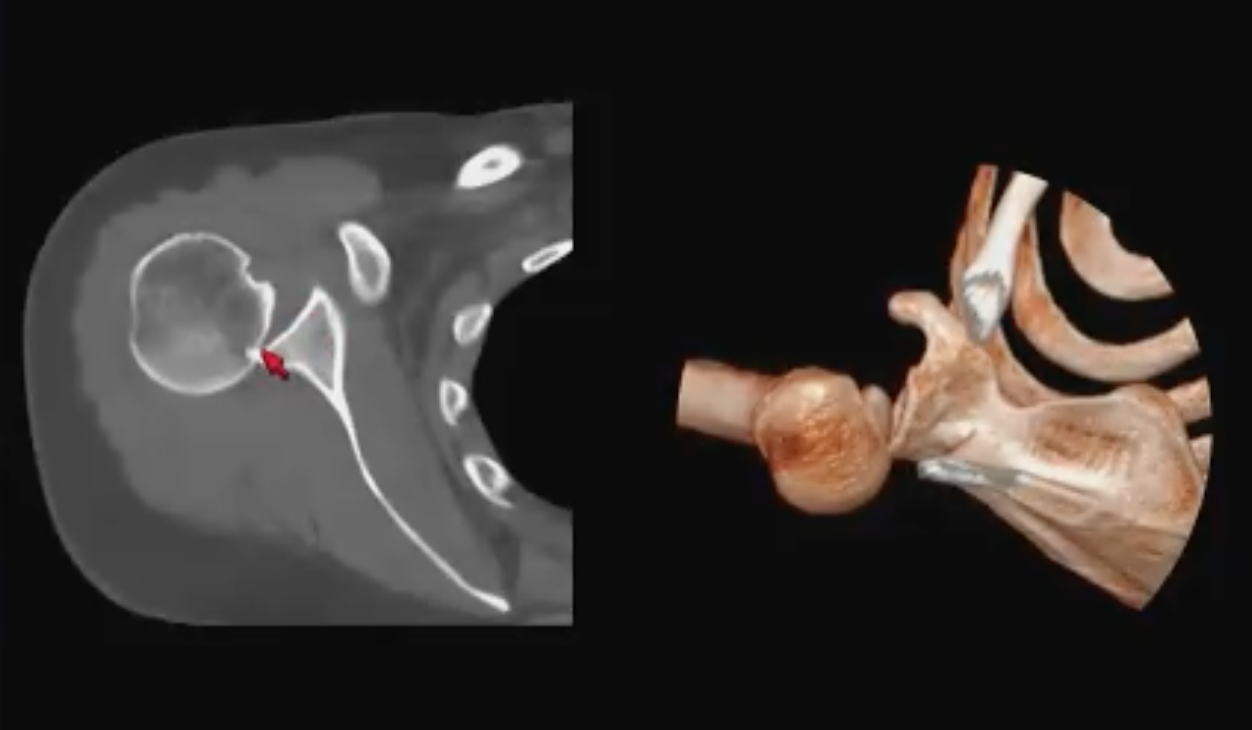 the patient could not the raise arm outside the field of view for the chest CT, so it got included and here we see that the humeral head impinged on the posterior glenoid, which is why the humeral head was lightbulb in appearance on the initial radiographs.”
the patient could not the raise arm outside the field of view for the chest CT, so it got included and here we see that the humeral head impinged on the posterior glenoid, which is why the humeral head was lightbulb in appearance on the initial radiographs.”
Scaphoid Fracture
The scaphoid is the most-commonly fractured carpal bone but 22% of clinically suspected scaphoid fractures are radiographically occult. “That is a problem because these tend to undergo osteonecrosis and avascular necrosis due to tenuous blood supply that’s retrograde, that goes from the distal pole to the proximal pole, frequently resulting in nonunion, that causes premature wrist osteoarthritis,” he explained.
The first three scaphoid fractures are arranged from easy-to-see to hard-to-see.
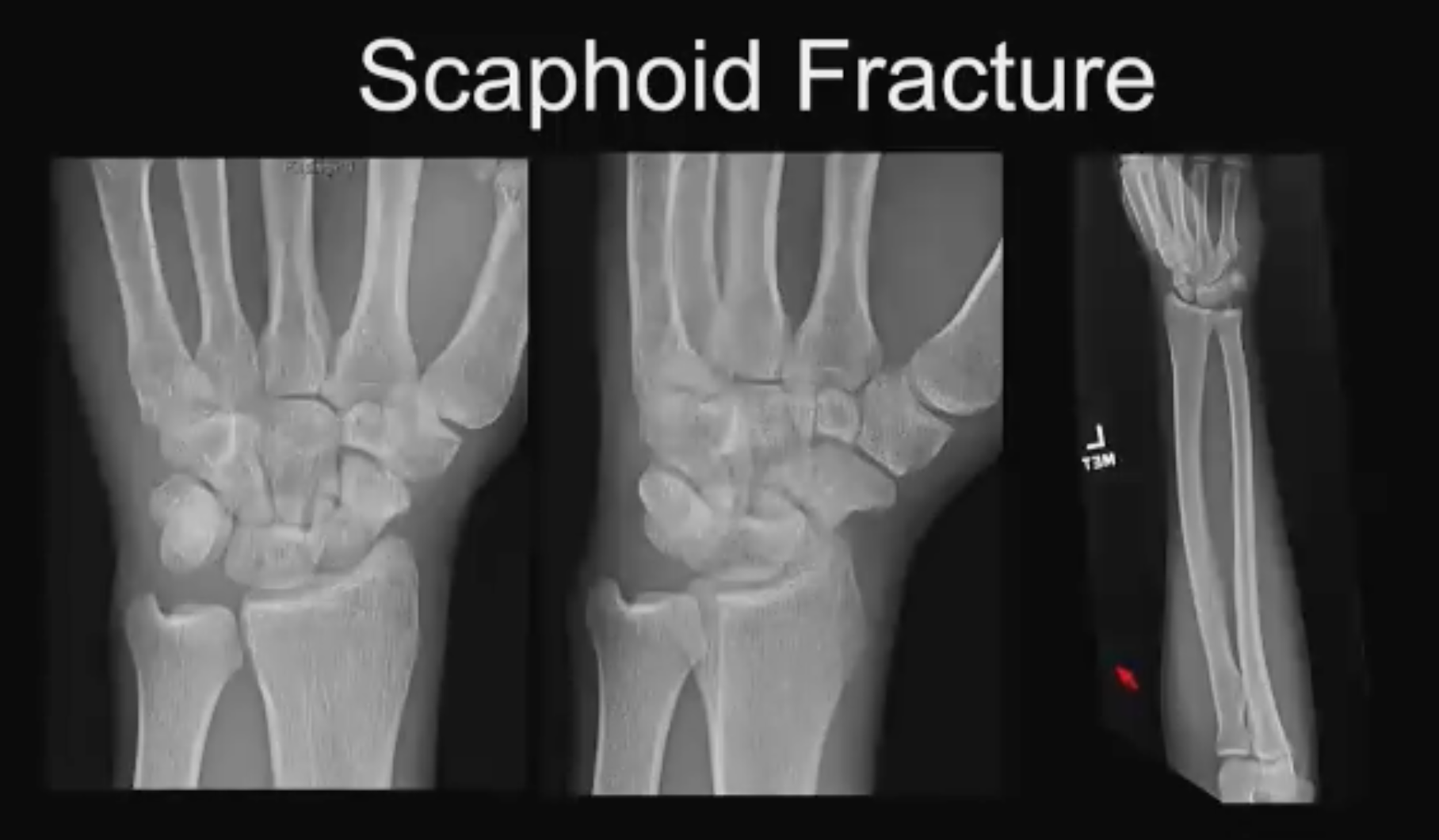
Scaphoid No. 1 (above). FOOSH Fall. “Most scaphoid fractures occur with a fall and an outstretched hand (FOOSH injuries),” said Dr. Asrani. “Often, we get a scaphoid waist fracture, which we can see nicely on this AP projection and even on this oblique view. Some can even be seen nicely on the forearm view. The center view shows a little bit of sclerosis, cortication along the edges. Therefore, this is a subacute to chronic fracture.”
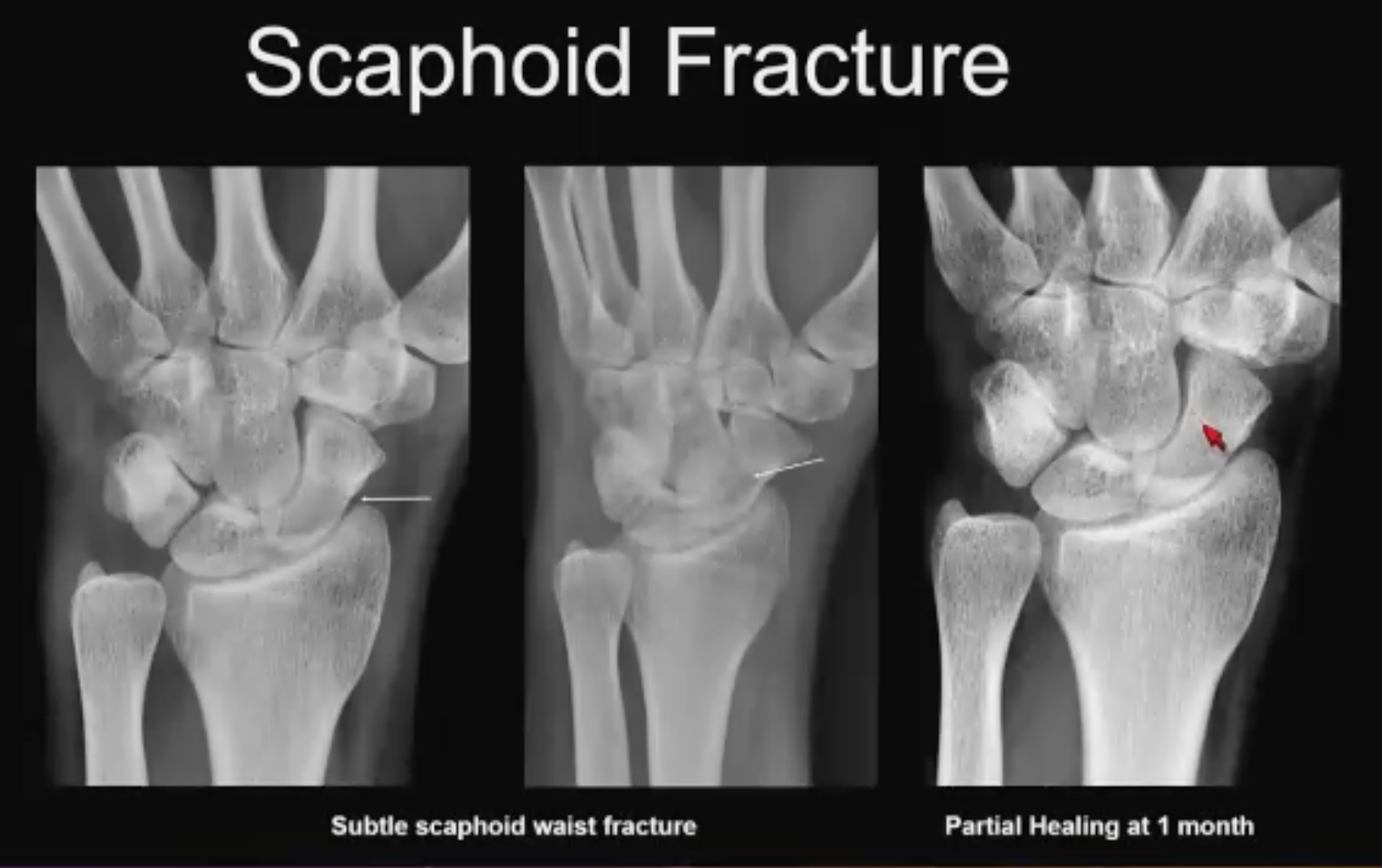
Scaphoid No. 2 (above). Subtle example. “You look at this at 2:30 AM, and you wonder, what is this? Is this a subtle line along the radial side? Then you look at the oblique view and the line going across and say, “maybe”. One month later you see that it has healed, thankfully, and it confirms your suspicion. This is a healing scaphoid fracture.”

Scaphoid No. 3 (above). Utility of the scaphoid view. “Include a scaphoid view in your series if you can—a scaphoid view is nothing but an ulnar deviation view, it elongates the scaphoid nicely, demonstrates the fracture nicely, and confirms the diagnosis. Include a scaphoid view in your wrist series in the ER.”

Scaphoid No. 4 (above). Radiographically occult, fall injury. “We’re looking at the AP view: There is a lot of osseus overlap here because of the forward flex position of the scaphoid. On the oblique view, we are not seeing anything. Patient has wrist pain, so you get an MR and there is this little T1 line through the waist of the scaphoid. On the sagittal PD sat-fat images, you see the fracture line very nicely. This is a radiographically occult non-displaced scaphoid fracture.”
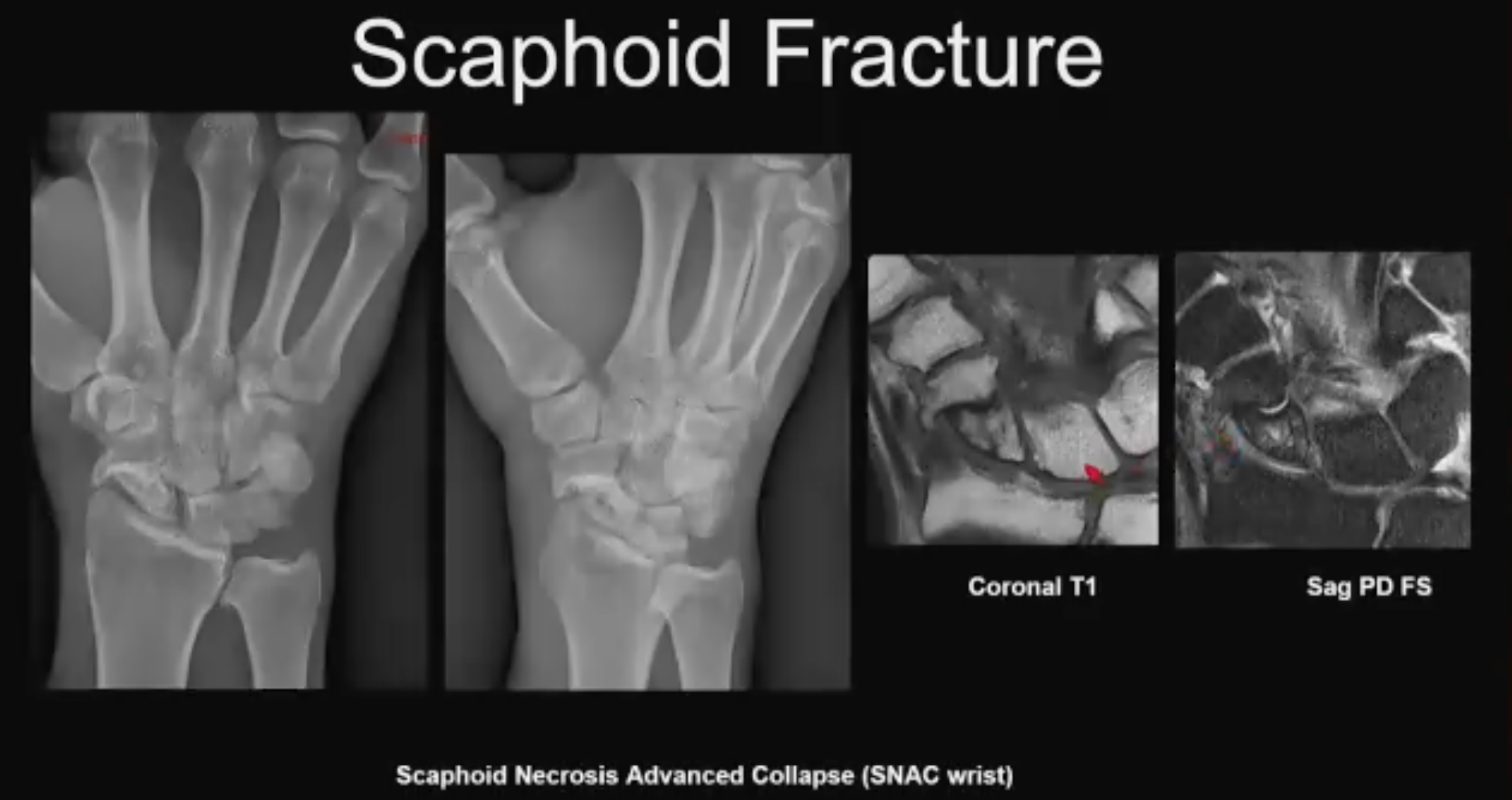
Scaphoid No. 5 (above). Chronic scaphoid fracture. “This is what happens if these scaphoid fractures get missed. This patient did not come in for treatment after the initial injury and several months to a year down the line came into the ER again with wrist pain. When you image this, you will see that there is pseudoarthrosis of the scaphoid waist fracture, early radio-carpal arthritis, a little bit of widening of the scaphoid interval. You do the MR and see there is loss of normal T1 signal. It’s a little patchy compared with other carpal bones with some T2 hyperintensity, so this is early osteo necrosis as well, and you see the arthritis very well. The fancy word for this is Scaphoid Necrosis Advanced Collapse (SNAC) wrist. This is a sequela of chronic scaphoid fracture, which will come through your ER as well.”
Lisfranc Fracture
"Up to a third of Lisfranc injuries are missed at initial presentation, and it’s a problem,” Dr. Asrani began. “Missed Lisfranc injuries result in chronic pain, disability, mid-foot arthritis, and certainly a lot of litigation.”
He provided some biomechanical perspective: Lisfranc was a surgeon in Napoleon’s army who discovered that if you amputate frostbitten soldiers’ feet at the tarsal-metatarsal articulation, it is a way to preserve the hindfoot and so this articulation was named after him, he explained. Dr. Asrani shared a photograph of footprints in the sand and noted that transmission occurs in the heel and the front of the foot. He described the column concept used to describe the mechanics of the forefoot: The medial column is formed by the first metatarsal; the second column is formed by the intermediate and the third cuneiforms with the second and third metatarsal; and the lateral column is the fourth and the fifth metatarsal with the cuboid.
sand and noted that transmission occurs in the heel and the front of the foot. He described the column concept used to describe the mechanics of the forefoot: The medial column is formed by the first metatarsal; the second column is formed by the intermediate and the third cuneiforms with the second and third metatarsal; and the lateral column is the fourth and the fifth metatarsal with the cuboid.
“The middle column is the most rigid with the most stability and the least amount of motion,” he said. “The second to fifth metatarsals are bound together with metatarsal ligaments, but there is no metatarsal ligament between the first and second metatarsal. Instead, we have this interosseus ligament that runs from the first cuneiform to the base of the second metatarsal, which is the Lisfranc ligament. Why is it important? Because the second metatarsal base acts like a keystone in the arch of the foot, and it is the most important structure. It provides the highest point and injuries to the base of the second metatarsal and the Lisfranc ligament can lead to collapse of the arch of the foot.”

Lisfranc No. 1 (above). 63-year-old patient w/neuropathy. The patient arrived at the ED with redness and swelling, with no memory of trauma. “We see there is lateral subluxation or dislocation of the tarsal-metatarsal articulation,” said Dr, Asrani. “This is the homo-lateral variety of Lisfranc fracture dislocation others being divergent. What happens in divergent is the first metatarsal stays where it is, and the rest move laterally. Here everything has moved laterally, and we see it very nicely on the AP and oblique radiographs, which can be compared with the frontal as well. This patient got a mid-foot arthrodesis. Some of you may think this is actually a Charcot foot, and that may be the case given her clinical presentation, especially since there is a school of thought that all Charcot foot’s start out as a Lisfranc ligament sprain.”

Lisfranc No. 2. Occult injury (above). 44-year-old patient w/foot pain after dance session. On the AP view: the second metatarsal lines end nicely with M2, the first metatarsal lines up nicely with M1, and the Lisfranc interval is congruous. Notes Dr. Asrani: “There is nothing to call. When you get a weight-bearing view, everything appears OK on cursory review until you examine the Lisfranc interval. It does look like the bases of the first and second metatarsal are slightly wider when compared to the right side.”
The pain persists so an MRI is obtained. “Loss of normal T1 signal in the medial cuneiform is compatible with fracture, which we see really nicely on the coronal PD fat-sat images,” he said. “There also is a sprain of the interosseous band and this patient required surgery. You want to be very careful about this interval, and if you are unsure get cross sectional imaging.”
Maissoneuve Fractures
The Maissoneve fracture is troublesome because the miss rate for a proximal fibular fracture at the first visit is between 14% and 44%. “You can potentially discharge a patient from the ER after a seemingly normal X-ray for an injury that actually needs surgical fixation,” Dr. Asrani cautioned.
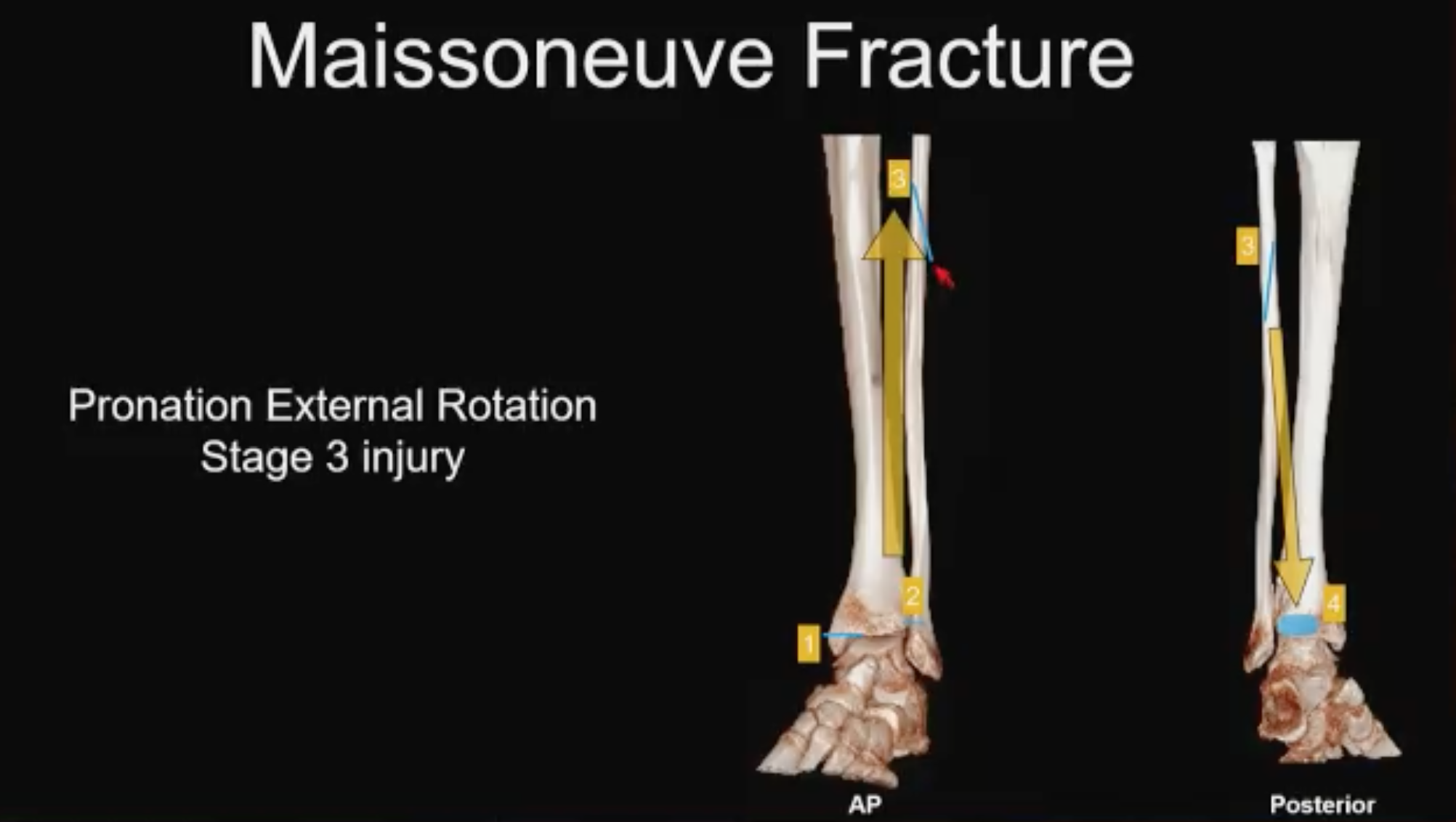
Maissoneuve No. 1 (above). Pronation external rotation, stage 3 Lauge-Hansen. Dr. Asrani explained: The foot starts off in pronation or eversion and rotates externally and that distracts the medial side of the ankle. Because it is typically a pull-off injury, you’ll get a transverse-oriented medial malleolar fracture or a deltoid ligament injury, the ligamentous equivalent. As the foot rotates externally, it takes out the anterior inferior tibiofibular ligament (AITFL) which tends to be radiographically occult most of the time; the force spirals up the interosseus membrane, rips the interosseus membrane and finally breaks through the proximal fibula. “What I want to highlight here is that when it gets to the fibula, it typically has a high anterior-low posterior configuration,” he explained, “because as the foot rotates externally the force typically comes down the back of the leg and takes out the posterior malleolus.”

Maissoneuve No. 2 (above). Fall on black ice, inability to bear weight. “When we look at the ankle radiographs, they look pristine, nicely done. Everything is congruent, no flex, no widening, nothing to suggest any bony injury,” said Dr. Asrani. “You are about to discharge the patient from the ER until you get the proximal tib-fib x-ray and you notice that high anterior-low posterior configuration with that spikiness that tells you it is an external rotation injury consistent with the Maissoneuve injury. It gets fixed with different types of hardware based on surgical preference.”
Compartment Syndrome
Compartment syndrome is a clinical diagnosis, not a radiological diagnosis to make, Dr. Asrani said. But the consequences of a miss are so devastating that he was compelled to highlight the condition for attendees. “Compartment syndrome is an ischemic state that develops after increased pressure develops in a tightly contained osteo-fascial compartment and a true orthopedic emergency seen in the ER,” he advised. “Tissue viability decreases over time and irreversible changes set in the muscle and nerves at 8 hours.”
Fracture is the most common cause, followed by blunt trauma, ad younger male patients are most at-risk. Tibial diaphysis (~36%), distal radius (~10%), forearm diaphysis (~8%) comprise the largest groups of compartment syndrome.
The clinical diagnosis is made from the 6 “p”s encountered in medical school training: pain out of proportion, pallor, poikilothermia, paresthesia, pulselessness, paralysis. However, most providers make the diagnosis using compartment manometry—if compartment pressure is within 30mm of the diastolic blood pressure, surgery is indicated. The role of imaging is to suggest presence of compartment syndrome or detect any complications.
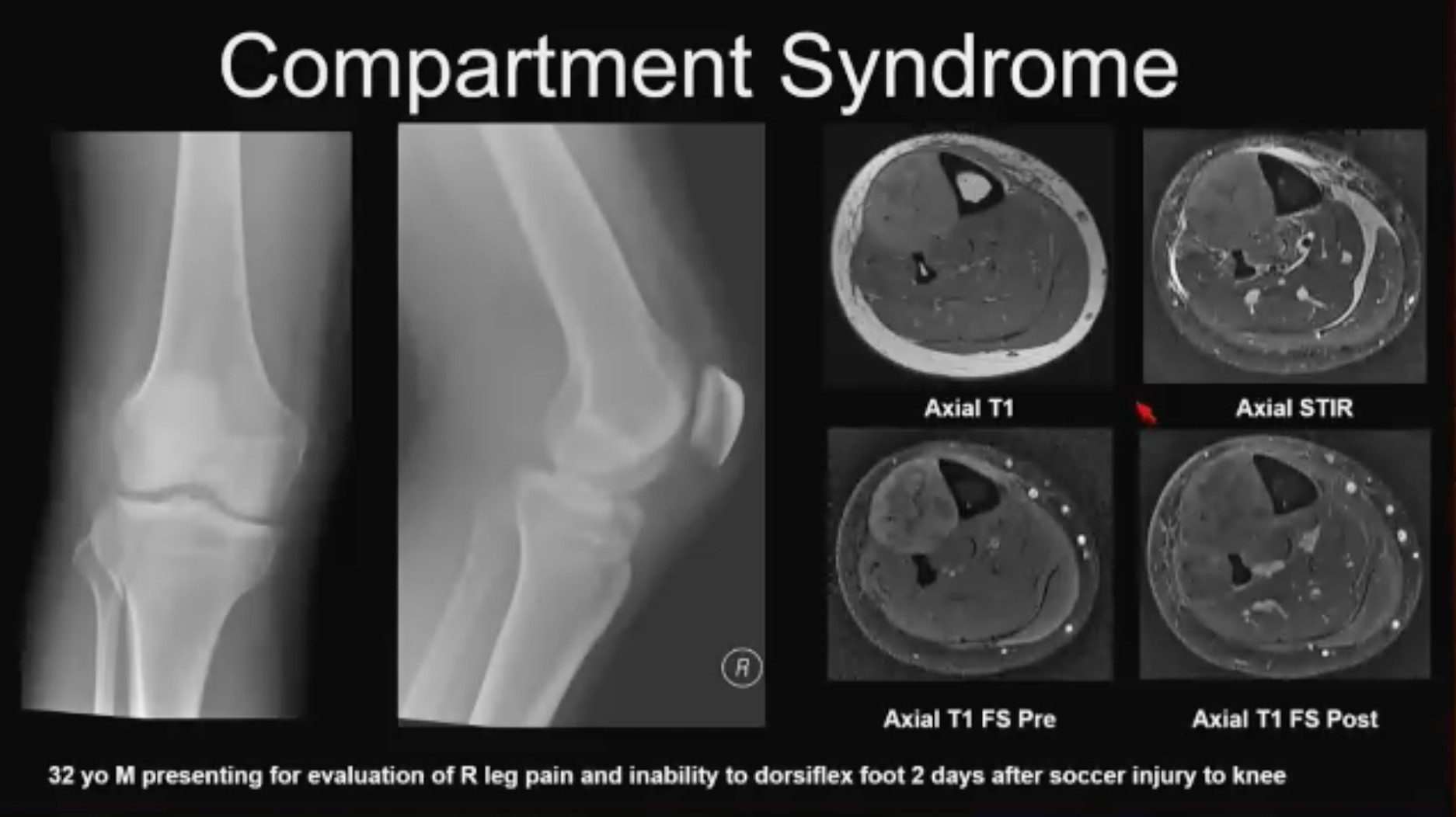
Compartment Syndrome No. 1 (above). 32-year-old soccer-playing patient w/knee injury. Patient did not seek treatment initially and arrived at ER a few days after injury occurred with inability to dorsiflex the ankle. Lateral tibial plateau fracture and knee joint effusion seen on x-ray and compartment syndrome was suspected. Compartment manometry showed normal pressure, so MR was acquired. Axial T1 images show a large anterior compartment that is slightly T1 hyper intense; a small T2 hyperintensity with a lot of fluid in the calf; and some stippling in the post contrast images suggestive of mild necrosis. This was a case of missed compartment syndrome and any surgical management was deferred at this point. Creatinine kinase level was elevated in this case.
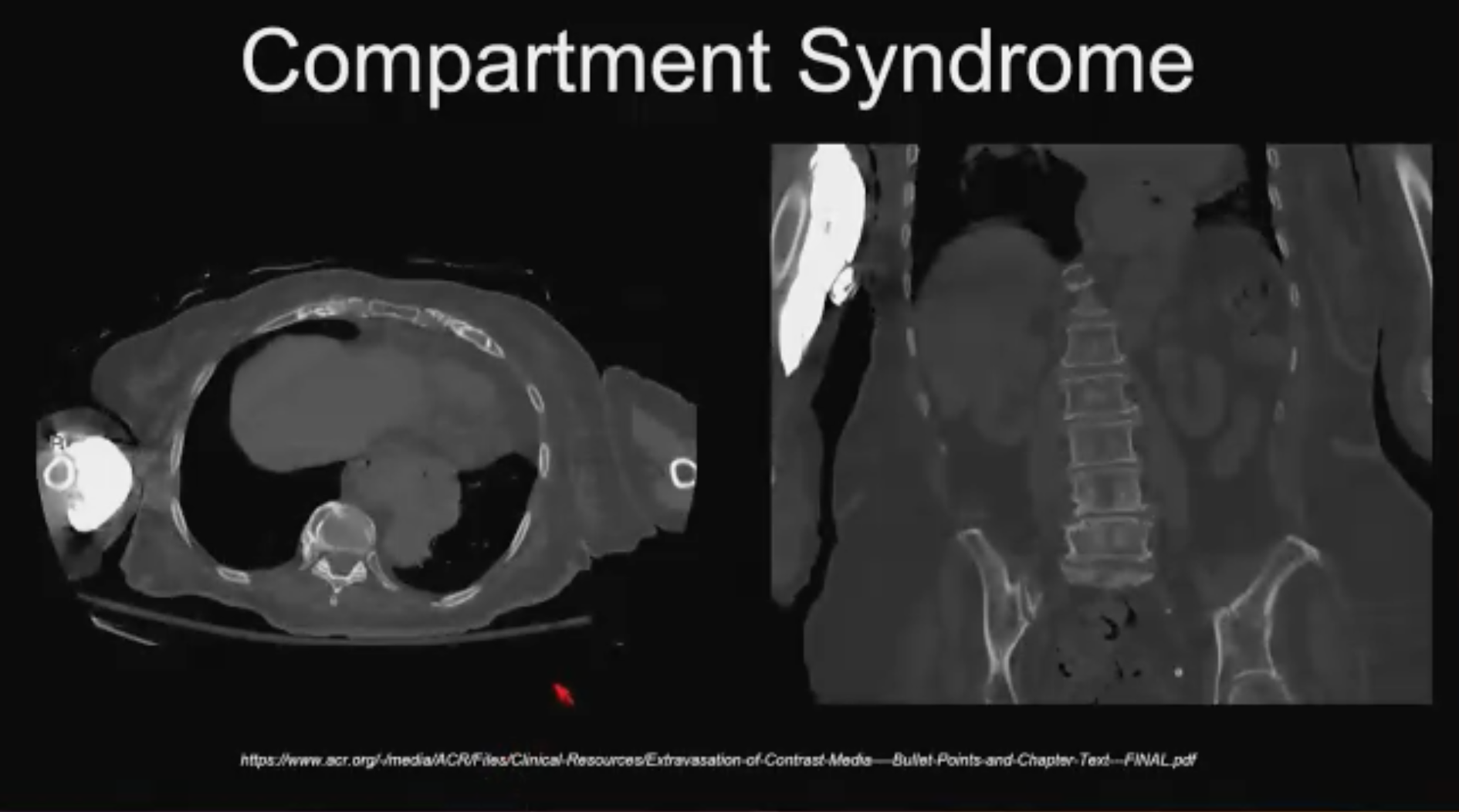
Compartment Syndrome No. 2 (above). CT contrast extravasation. “This is the compartment syndrome that you might encounter as you are starting to take call in the ER,” Dr. Asrani said. “With the large volumes of CT contrast that we use these days, they can extravasate and they can infiltrate but the good news is that most of the contrast we use is low osmolar and compartment syndrome is extremely rare. Do your clinical exam and have a low threshold for surgical consultation.”
Dr. Asrani left attendees with these 5 take-home points to help radiologists sleep easy:
• Posterior Shoulder Dislocation: Remember the light bulb humeral head and trough sign
• Scaphoid Fracture: obtain scaphoid view; have a low threshold for MRI
• Lisfranc Fracture Dislocation: assess MT (metatarsal) cuneiform alignments, low threshold for • CT/MRI if pain is persistent and negative x-rays
• Maissoneuve Fracture: know the mechanism and obtain tib-fib x-ray
• Compartment Syndrome: suspect when compartment size is asymmetrical
Hub is the monthly newsletter published for the membership of Strategic Radiology practices. It includes coalition and practice news as well as news and commentary of interest to radiology professionals.
If you want to know more about Strategic Radiology, you are invited to subscribe to our monthly newsletter. Your email will not be shared.