On a daily basis, we are seeing things that are very surprising.
Judith K. Amorosa, MD, FACR, is clinical professor of radiology, Robert Wood Johnson Medical School, and a thoracic radiologist with University Radiology Group in New Brunswick, NJ, which is currently feeling the storm of community spread. In her portion of the Covera Health webinar, “Managing Covid-19 on the Front Lines,” she described the radiological features of coronavirus onset over time, providing context for advisories and consensus statements from ACR, Society of Thoracic Radiology, and RSNA, stating that chest CT is non-specific for screening or diagnosing Covid-19.
On March 11, the ACR issued a recommendation that chest CT not be used to screen or diagnose the presence of Covid-19 infection. The college updated its recommendation on March 22 in response to requests to use chest CT in the absence of testing resources, urging caution in stating that a normal chest CT does not preclude the presence of Covid-19, but recognizing that decisions could be impacted by locally constrained resources.
ACR’s advisory did urge radiologists to be aware of the CT appearance of Covid-19 in order to identify findings consistent with infection in patients imaged for other reasons. “On a daily basis, we are seeing things that are very surprising,” said Dr Amorosa, sharing a bar chart from a paper published in Radiology that illustrated the stealthy progression of the disease (see Figure).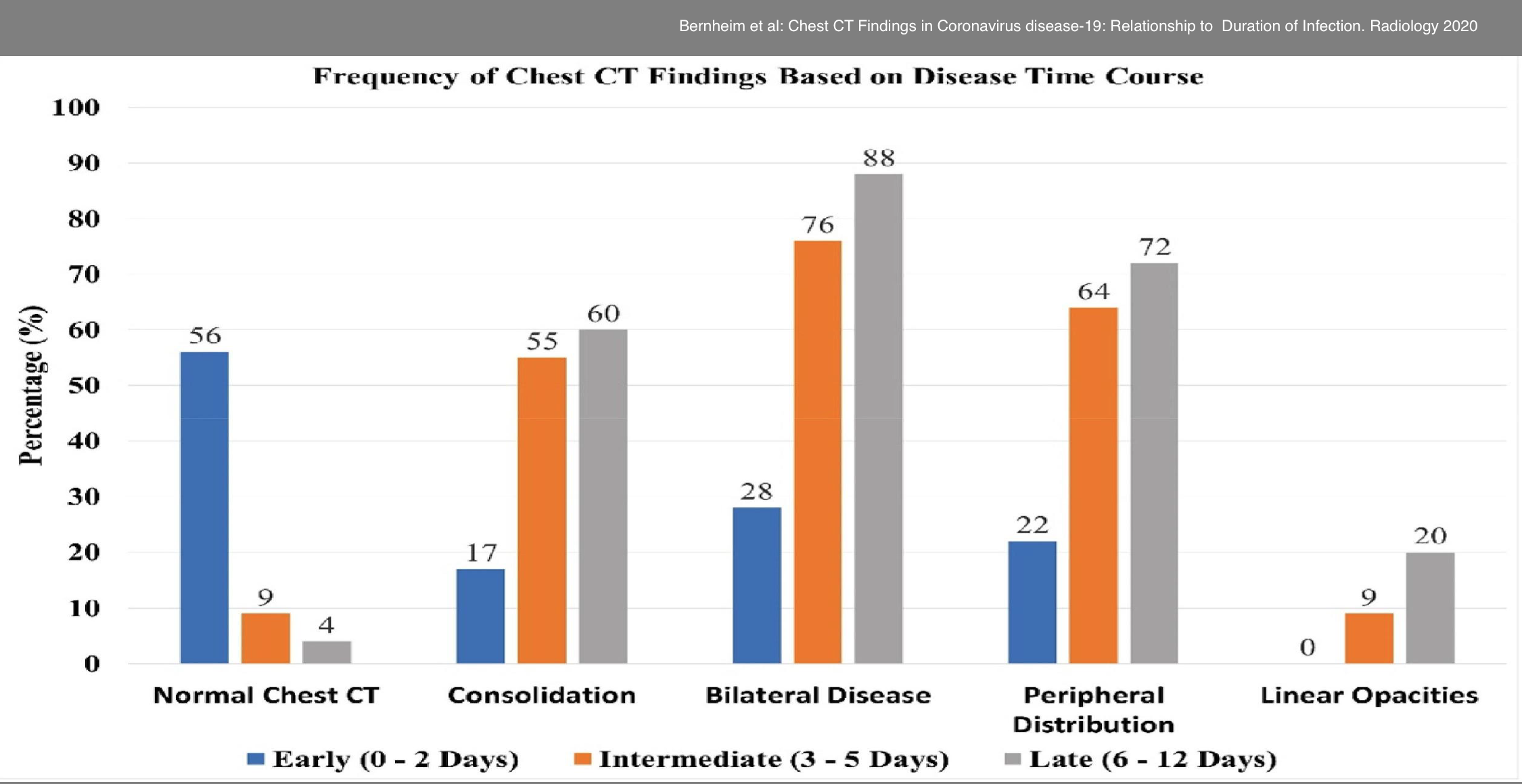
Her first close look at the CT signature of Covid-19 came during a virtual visit to the recent annual meeting of the Society of Thoracic Radiology in Indian Wells, CA, where Jeffrey Kanne, MD, University of Wisconsin, and Michael Chung, MD, Icahn School of Medicine, Mount Sinai, MT, presented, “A Covid-19 Update for the Radiologist.” Since then, she has seen many cases from her vantage point in Central New Jersey.
A Gathering Storm of Findings
Patients in the Bernheim et al study were categorized based on the number of days between symptom onset and CT: early stage (0-2 days), intermediate stage (3-5 days), and late stage (6-12). In CTs acquired in the early stage of disease progression, more than 50% of the CT are considered normal; but just 3-5 days from symptom onset, only 9% are considered normal; and in the late stage, 4% were considered normal. Likewise, other key disease findings dramatically increased over time—consolidation, bilateral disease, peripheral distribution, and linear opacities. Findings associated with disease progression are:
Dr Amorosa’s overview included the following additional CT findings:
Additionally, 76% of the CT findings on patients that tested positive were peripheral; 78.7% were multilobar; 38% involved all 5 lobes; and 80% were posterior.
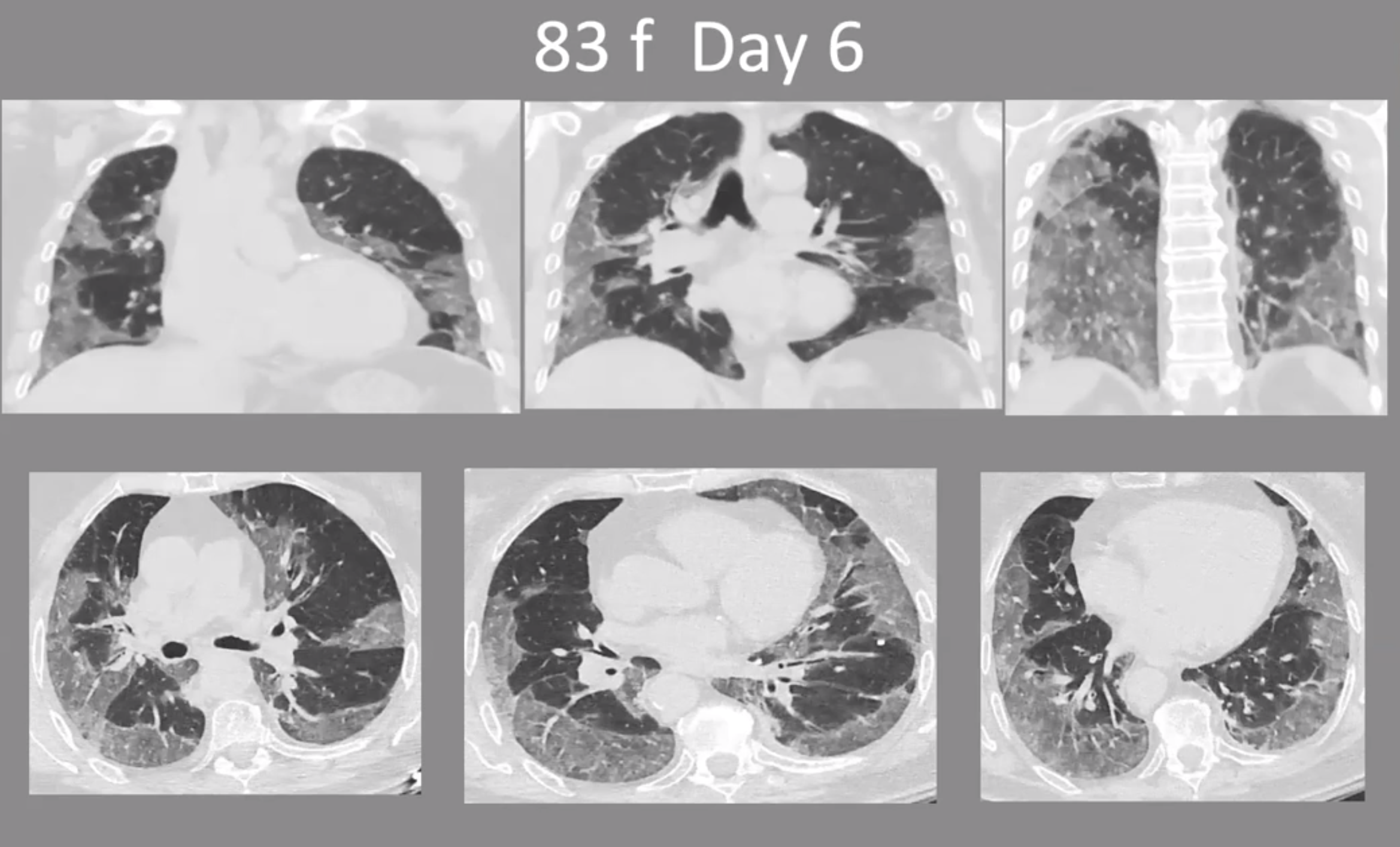
The cases shared by Dr. Amorosa during the webinar exhibited a dramatic proliferation of findings in the lung between a patient’s early stage CT and intermediate and late-stage CT. She described the CT of an 83-year-old female patient on day 1 as almost normal with the exception of minor ground glass opacities. By day 6, the same patient is severely symptomatic. “Look what has happened,” she said. “The CT is quite abnormal with all of these ground glass peripheral opacities literally surrounding the lungs and within the lung.” (See Figures).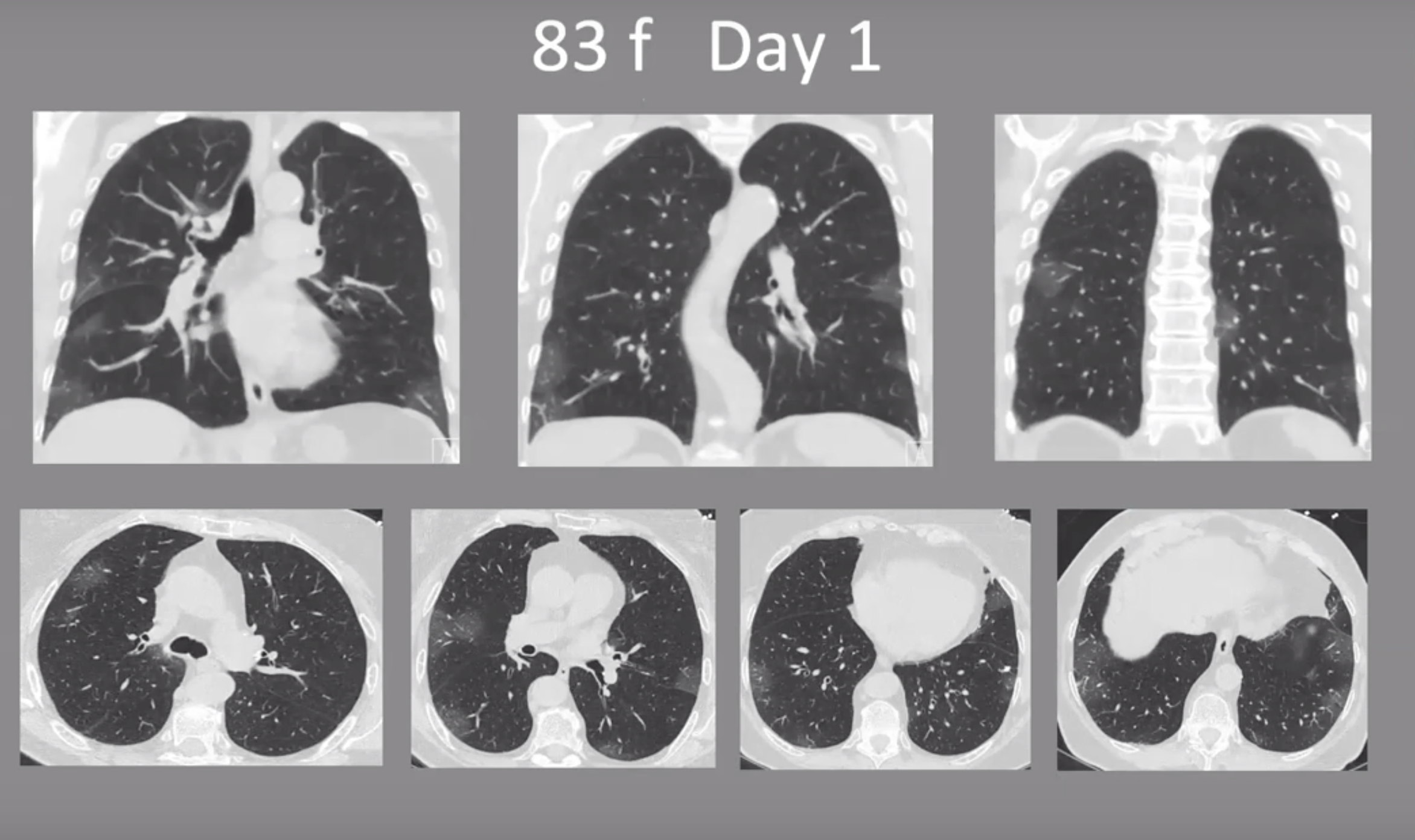
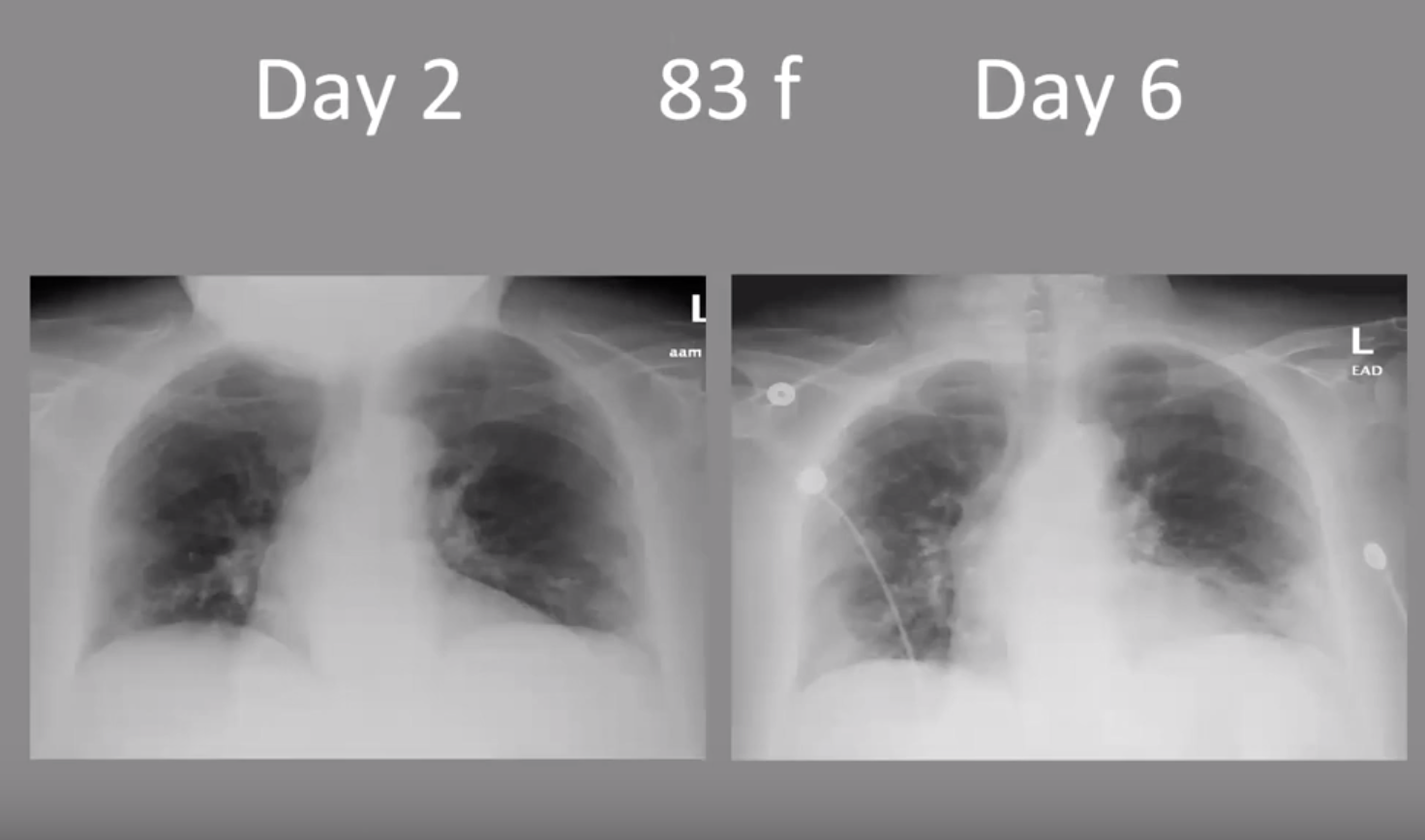
She also pointed out that x-rays of the same patient on Day 2 and Day 6 were not signficiantly different or as descriptive as the CTs for visualizing disease progression (see Figure).
In scrolling through a series of cases of patients from 25-years-old to 83, Dr. Amorosa pointed out various patterns, including the Atoll (a reverse halo) and crazy paving, which she likened to European streets cobbled with different-sized stones. “It’s important that the technique be such that you have thin slices and are able to look at all of the pattern.”
What Do You Do?
Is chest CT appropriate for initial evaluation and follow-up of coronavirus? Neither the STR, ACR, RSNA, or Dr. Amorosa recommend using CT to diagnose or follow Covid-19.
STR, ACR, and RSNA all recommend against the use of CT for frontline screening or diagnosis of cornonavirus, primarily because the findings on chest imaging are non-specific to Covid-19. Advises the ACR: “Generally, the findings on chest imaging in Covid-19 are not specific, and overlap with other infections, including influenza, H1n1, SARS, and MERS. Being in the midst of the current flu season with a much higher prevalence of influenza in the US than Covid-19, further limits the specificity of CT.”
The STR Covid-19 position statement, issued on March 11, mentions two other considerations: a normal chest CT does not exclude COVID-19, and getting a patient into a CT has a high degree of difficulty.
“There are so many other entities that can look like this, it is hard to be absolutely specific that Covid-19 is what the abnormality on CT is due to,” Dr. Amorosa concluded. “It should not be used to screen or diagnose the virus because it is non-specific.”
She acknowledged the contributions of colleagues Mark Bramwit, MD, F Kang, MD, and Murray Becker, MD.
Hub is the monthly newsletter published for the membership of Strategic Radiology practices. It includes coalition and practice news as well as news and commentary of interest to radiology professionals.
If you want to know more about Strategic Radiology, you are invited to subscribe to our monthly newsletter. Your email will not be shared.